Introduction To Total Joint Replacement And Rehabilitation
Undergoing a total joint replacement is a significant step towards regaining your active lifestyle, reducing pain, and increasing mobility when conservative treatments are no longer effective. Whether you are contemplating a hip, knee, or shoulder replacement, understanding the journey ahead—especially the role of rehabilitation—is essential for the best possible joint replacement recovery. At Bull City PT, we are here to guide and encourage you throughout each stage of your recovery process as you reclaim your independence and return to doing the activities you love.
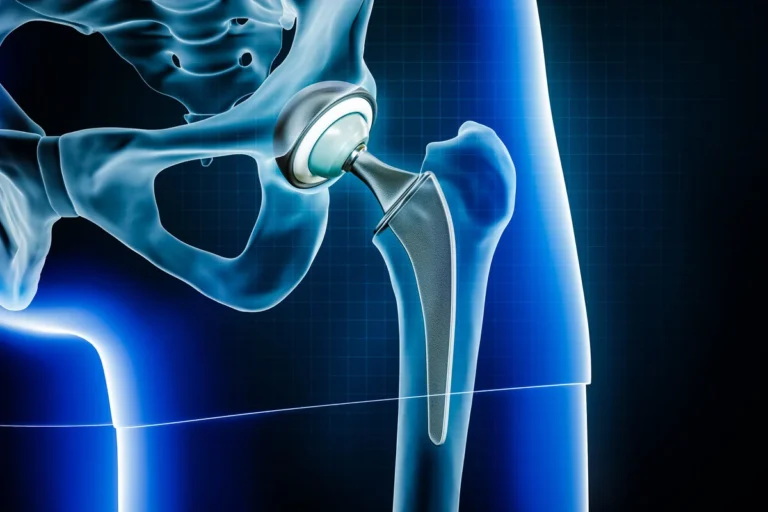
A total joint replacement involves removing damaged or diseased parts of an arthritic joint and replacing them with specially designed prosthetic components. Most commonly performed on the hips and knees, these surgeries can also benefit shoulders, ankles, and elbows. The procedure can significantly relieve pain, restore function, and improve your quality of life—but only when it’s paired with a comprehensive and dedicated rehabilitation plan.
Why Total Joint Replacement Rehabilitation Matters After Surgery
Rehabilitation is not just a supplementary phase following surgery—it’s a fundamental component of a successful recovery. The immediate post-operative period is critical for optimizing your joint’s healing and function. Early recovery, which involves initiating rehabilitation activities such as physical therapy and gentle exercises soon after surgery, is essential for promoting healing, improving strength, and facilitating a faster return to daily activities. Structured, safe movement helps reduce stiffness, strengthen supportive muscles, and eventually, restore balance, flexibility, and full motion. Without rehabilitation, you run the risk of slower recovery, persistent pain, decreased mobility, and complications such as stiffness or weakness.
Goals Of Post-Operative Recovery And Physical Therapy
Your primary goals after joint replacement are to manage pain, prevent complications, restore range of motion, and rebuild strength. Early mobility is encouraged by your care team, with the aim of returning you to day-to-day activities and, eventually, the recreational pursuits that bring you joy. Physical therapy provides you with individualized exercises and expert attention to support safe and effective progress in each unique recovery phase.
What To Expect In This Guide
This comprehensive article will walk you through every step of the joint replacement recovery process. We’ll explore evidence-based exercise guidelines, timelines for rehabilitation, what to expect during physical therapy sessions, and how to set realistic, motivating goals. No matter where you are in your journey—from your first steps after surgery to years down the road—Bull City PT is dedicated to offering encouragement, education, and hands-on support for lifelong joint health.

What Are The Exercise Guidelines For Joint Replacement?
Exercise plays a vital role in the recovery process after total joint replacement. Following a standardized set of exercise guidelines for joint replacement ensures you regain strength, mobility, and confidence while minimizing risk. It is important to understand when and how to begin exercising, as well as which activities are best suited for each stage of rehabilitation. Patient-specific factors, such as age, overall health status, and the type of joint replacement, play a significant role in determining the most appropriate exercise guidelines and rehabilitation process. Working closely with a skilled physical therapist, like those at Bull City PT, sets the foundation for a safe and successful recovery.
General Principles For Safe Exercise After Joint Replacement
The cornerstone of rehabilitation protocols after joint replacement is gradual, progressive movement that encourages healing without causing harm. Early on, focus on gentle, pain-free movements aimed at restoring flexibility and reducing swelling. Simple exercises such as ankle pumps, quad sets, and gentle range of motion movements are typically introduced within the first few days post-surgery. As healing advances, the emphasis shifts toward increasing joint mobility and muscle strength through carefully selected, progressively challenging exercises. Building endurance through consistent activity is also important, as it supports overall recovery and helps maintain long-term joint health. Always prioritize proper form, avoid high-impact activities, and stop any exercise that causes sharp or unusual pain.
When And How To Start Exercise Post-Surgery
Exercise can begin as soon as you have medical clearance, which is commonly within 24 hours post-operation for most joint replacements. Early movement helps prevent complications such as blood clots and joint stiffness. Physical therapists guide initial movements, ensuring you maintain safe positioning and avoid motions that could put your new joint at risk. A randomized controlled trial has shown that early, supervised exercise significantly improves functional outcomes after joint replacement. At Bull City PT, we tailor activity plans to match your surgery and health status, so you gain confidence while respecting any post-op restrictions.
Precautions And Contraindications
It’s essential to be mindful of precautions unique to your specific joint replacement. For example, after hip replacement, certain twisting or bending motions may be restricted. For knee replacements, avoid kneeling or high-impact bending in the early weeks. Always follow your therapist’s advice about weight-bearing limitations and movement restrictions, as failing to do so may slow recovery or even threaten the success of your implant. Monitoring limb length and addressing any discrepancies is also important after surgery to prevent complications and ensure optimal rehabilitation.
Role Of A Physical Therapist In Guiding Exercises
Physical therapists are your partners throughout the physical therapy joint replacement recovery process. They assess your progress, ensure exercises are performed correctly and safely, and modify routines as you heal. This personalized attention helps you meet milestones faster, manage discomfort, and prevent setbacks or complications. Bull City PT’s therapists specialize in post-joint replacement care, offering the encouragement, expertise, and support you need at every step.
Progression Of Exercises Through Different Recovery Phases
Exercise after joint replacement typically progresses through several phases. The initial focus is on basic mobility and gentle strengthening. As healing progresses, your therapist will introduce more challenging exercises, such as step-ups, resistance band movements, or balance activities, tailored to your individual recovery timeline. Some advanced exercises may involve lifting more weight or increasing resistance to further enhance strength and stability. Eventually, your program will include advanced movements that mimic daily activities—climbing stairs, rising from a chair, or walking on uneven surfaces—helping you transition back to full independence and your favorite activities.
By following evidence-based rehabilitation protocols and the personalized guidance of Bull City PT’s expert therapists, you can confidently navigate each phase of your joint replacement recovery. Remember, consistency and safety are key—listen to your body, keep open lines of communication with your care team, and celebrate each victory along the way!
Physical Therapy After Total Hip Replacement: Timelines And Milestones
How long do you need physical therapy after total hip replacement? Most patients benefit from a structured physical therapy hip replacement program for about 8 to 12 weeks after surgery, although your timeline may vary depending on personal progress, health factors, and your surgeon’s guidance. Initial supervised therapy often transitions to independent exercise as you build confidence and achieve functional goals. Your recovery timeline is unique, and dedicated support from your physical therapist ensures you progress at the right pace while reducing the risks of complications and setbacks.
The journey to full mobility following a total hip replacement starts the moment you leave the operating room. Physical therapy provides the framework, expertise, and encouragement needed to restore your independence and return to an active lifestyle. Reaching milestones at the right time supports not only joint health but also your overall well-being, which is why following a personalized recovery timeline after hip replacement is so critical.
Hip abduction exercises play a key role in strengthening the hip muscles after total hip replacement. Targeting the hip muscles through hip abduction, especially with exercises like standing hip abduction, helps improve stability, mobility, and overall function. Standing hip abduction is commonly included in rehabilitation protocols to enhance hip muscle strength, support safe movement, and reduce the risk of dislocation during recovery.

Typical Duration Of Therapy After Hip Replacement
After a hip replacement, you can expect outpatient or home-based physical therapy hip replacement sessions 2-3 times per week for the first 4 to 6 weeks, with gradual reduction in frequency as functional milestones are achieved. Most active adults see significant gains in strength, flexibility, and balance within the first 3 months, but some may need ongoing therapy for up to 6 months, especially if there are complications or pre-existing conditions. Your commitment to attending therapy and doing prescribed home exercises helps shorten recovery time and optimize outcomes.
What Are The Key Milestones After Hip Replacement?
Reaching certain hip replacement rehab milestones can serve as a powerful motivator. At the 2-week mark, many patients are able to move more easily with an assistive device, manage pain better, and begin gentle range-of-motion work. By 3 months, you’re typically walking without aid, handling daily tasks, and rebuilding muscle strength. At 1 year, your new hip should support even more activities—some patients return to hiking, cycling, or swimming by this stage. These timelines are guidelines, so don’t be discouraged if yours is a bit different.
Factors Affecting Your Recovery Timeline
Your recovery timeline for hip replacement is affected by factors like age, underlying health conditions (such as diabetes, obesity, or cardiovascular disease), preoperative strength, and the specific type of hip replacement procedure you received. Complications like infection, delayed wound healing, or issues with the new joint also play a role in determining how long therapy may be needed. Regular check-ins with your Bull City PT physical therapist and your orthopedic surgeon allow your plan to be tailored exactly to your current needs and progress.
When Is Extended Or Additional Therapy Needed?
Some individuals may need extended or recurring therapy if they experience persistent pain, difficulty walking, notable muscle weakness, or issues with balance. If you feel your progress has plateaued or new problems arise, don’t hesitate to request a re-evaluation. At Bull City PT, we’re committed to empowering you through every stage of recovery and will adjust your program as needed for your best outcome.
Transitioning To Independent Exercise
As you achieve your early mobility and strength milestones, there will be a natural transition from supervised, in-clinic sessions to a safe and effective independent exercise routine. Your therapist at Bull City PT will educate you on the appropriate home exercises, ensure you have proper form, and provide encouragement for maintaining your gains after formal therapy concludes. Long-term success hinges on remaining active and integrating exercises into your everyday life while being mindful of any warning signs.
Whether you’re just starting out or advancing through your milestones, Bull City PT in Durham and Brier Creek is here to guide you at every phase of your hip replacement recovery, celebrating your achievements and supporting your journey to lifelong mobility.
Total Hip Replacement Exercises After 2 Weeks
Two weeks after your total hip replacement, you are entering a crucial phase of early rehab focused on steady progress, safety, and setting the groundwork for future strength and mobility. While your mobility will still be somewhat limited, this period is all about easing swelling, gently restoring range of motion, reactivating your muscles, and developing confidence with assistive devices. Your main priority should be moving with purpose and caution as you build strength and mobility—remember, every small step you take now supports your long-term recovery.
What Are The Goals Of Exercise At This Early Post-Op Stage?
The primary objectives of the first phase of hip replacement exercises are to prevent complications like blood clots, reduce swelling, improve circulation, and begin restoring both function and range of motion around your new joint. Just as important is re-engaging the muscles surrounding your hip—especially your quadriceps, glutes, and core—so they can support your movements safely. Finally, early exercise helps you become comfortable moving with crutches, a walker, or a cane as needed.
Setting realistic expectations is key; you are not striving for major accomplishments yet, but for daily consistency. Focus on small improvements—such as greater comfort during activities of daily living—which lay the foundation for advanced activities in later stages.
What Are Sample Exercises You Can Do After 2 Weeks?
Your physical therapist at Bull City PT will tailor a specific plan for your needs, but most people, after two weeks since their total hip replacement, can safely perform gentle, low-resistance activities, including:
- Ankle pumps: From the starting position lying on your back with feet flat on the floor, flex your ankles up and down, lifting your foot and then slowly lowering it to stimulate blood flow and prevent clotting. Maintain tension in your lower leg muscles throughout the movement.
- Quad sets: Begin in the starting position with your right leg or left leg straight and foot on the floor. Gently tighten your thigh muscles by squeezing and holding for 5-10 seconds, then slowly return to the starting position. Keep your arms relaxed at your sides.
- Gluteal squeezes: While lying down with knees bent and feet flat on the floor, tighten your buttock muscles by squeezing them for a few seconds at a time, then slowly return to the starting position. Maintain tension in your glutes during the squeeze.
- Gentle heel slides: Start lying on your back with both feet flat on the floor and knees bent. Slowly slide your right heel or left heel toward your buttocks, bending your knee, then slowly return your foot to the starting position. Keep your arms at your sides and maintain tension in your leg muscles.
- Assisted knee bends: If permitted, begin with your knees bent at a right angle and feet flat on the floor. Use your arms to gently assist in bending your right leg or left leg, focusing on controlled movement at the knee and hip. Never force the motion, and slowly return to the starting position.
Your therapist will monitor you closely for correct form, including proper arm and elbows positioning, chest alignment, and optimal repetition based on your healing rate. These exercises are usually performed two to three times a day, with the hope of increasing frequency and complexity as you progress.

How Much Weight-Bearing Is Allowed, And What Assistance Devices Should Be Used?
Most patients are encouraged to put some weight on their new hip—what’s called weight-bearing as tolerated (WBAT)—but your physician and physical therapist will clarify your individualized instructions. Many adults use a walker or crutches at this stage, which provide both support and safety. Gradually, with improved strength and confidence, you may transition to a cane. It’s key to practice your prescribed gait pattern to avoid developing poor movement habits.
How Do You Manage Pain And Discomfort During Exercises?
Mild discomfort is to be expected, but you should never push through sharp pain or significant swelling. Use strategies such as pre-exercise icing, scheduling pain medication per doctor’s instructions, and pacing yourself with adequate rest between sessions. Listen to your body—if you feel excessive fatigue, bleeding, or fever, stop and inform your PT immediately. At Bull City PT, our therapists monitor your pain and customize your program to promote comfort and confidence every step of the way.
What Precautions Help You Avoid Hip Dislocation After Surgery?
Protecting your new hip from dislocation is vital, especially during this early stage. Common precautions often include avoiding low seats, twisting your operated leg inward or outward, crossing your legs, or bending your hip beyond 90 degrees. Your therapist will guide you through every movement—whether getting out of bed, rising from a chair, or basic hygiene activities—ensuring that safety remains your highest priority. When in doubt, always move slowly and ask for help.
Early progress can be encouraging and empowering. At Bull City PT, our team is dedicated to providing you with hands-on guidance and emotional support, helping you gain confidence and independence. With patience and persistence in your early rehab hip replacement journey, you’ll be well on your way to long-term success!
Exercises For Hip Replacement After 3 Months And Beyond
Reaching the three-month mark after your hip replacement surgery is an exciting milestone. By this stage, most active adults can look forward to progressing from basic recovery to more functional and strengthening after hip surgery exercises. At Bull City PT, we’re here to help you regain mobility, build confidence, and safely re-engage with the activities you love.
What Types Of Exercises Should I Do After Hip Replacement At 3 Months?
At this stage, exercises focus on increasing strength, flexibility, balance, and functional mobility. Safe, progressive activities now include step-ups with proper form, side-leg raises, and standing marches. Resistance band exercises are especially beneficial, helping to rebuild hip and lower limb strength without compromising your new joint. You may also begin stationary cycling and pool-based exercises (if cleared by your physical therapist) for low-impact cardiovascular benefits. Remember, consistency and good technique are more important than intensity.
Sample Exercises For Intermediate Hip Replacement Recovery
Your Bull City PT specialist will create a tailored routine, but here are some examples:
- Step-Ups: Step up onto a low platform with your operated leg, then step down. Repeat 10-15 times, gradually increasing height as strength allows.
- Resistance Band Abductions: Secure a resistance band around your ankles. Gently move your surgical leg out to the side, keeping your hips level. Repeat 2-3 sets of 10-12 reps.
- Mini-Squats: Stand with feet hip-width apart and gently bend knees, keeping your hips and knees aligned. Hold a countertop for balance, if needed.
- Balance Activities: Stand on your surgical leg for up to 30 seconds, progressing to closed-eye or unstable surface variations as able.
When Can I Return To Work, Driving, Or Recreational Activities After Hip Replacement?
Most individuals can safely return to desk jobs and driving at this point, provided they have adequate hip mobility, strength, and reaction time. Manual labor or high-impact sports may require a longer transition. Recreational activities such as walking, swimming, golfing, and gentle cycling can often be gradually reintroduced under guidance. Always consult your Bull City PT therapist before resuming any demanding pursuit—together, you’ll plan the safest and most effective return-to-activity timeline.
How Can I Monitor For Setbacks Or Complications After Progressing In Rehabilitation?
Stay watchful for new or worsening pain, increased swelling, joint warmth, or difficulties with movement—these may signal a complication or overuse. Communicate promptly with your therapist or orthopedic team if you notice persistent issues. Periodic check-ins with your provider, even if you’re feeling well, help ensure your recovery is on track and prevent minor problems from becoming major setbacks. Remember, the journey back to full function should be steady and supportive; don’t rush, and listen to your body’s signals.
Most importantly, celebrate your progress! Every step, squat, and stair climbed is a testament to your dedication and the power of guided rehabilitation. At Bull City PT, we’re with you for every milestone of your journey—helping you move with confidence for years to come.
Exercises For Hip Replacement After 1 Year: Maintaining Mobility And Strength
One year after your hip replacement, it’s essential to shift focus from immediate post-surgical recovery to long-term lifetime joint care. At this stage, you’ll want to maintain—and even improve—mobility and strength so that your new joint serves you well for years to come. The exercises and habits you develop now are key in preventing future problems, supporting active aging, and maximizing your quality of life. With Bull City PT’s encouraging, personalized approach, you’ll find it possible (and enjoyable) to stay fit, confident, and independent.
What Exercises Should I Do One Year After Hip Replacement?
One year post-surgery, most patients can safely engage in a broad spectrum of physical activities. Focus on recommended long-term exercise routines such as brisk walking, swimming, cycling (stationary or outdoor), low-impact aerobics, and gentle hiking. These activities support cardiovascular health, enhance flexibility, and maintain joint lubrication. In addition, continue to include a structured strength training routine—two to three times a week—targeting the glutes, quads, hamstrings, and core. Resistance bands, light weights, or bodyweight movements (such as squats, bridges, and step-ups) are safe and effective options. Pilates, yoga, and balance exercises (like standing heel raises or single-leg stands) are excellent for joint stabilization and overall function. If you enjoy group exercise, consider joining a class designed for active adults or those at similar life stages. Remember, it’s important to avoid high-impact or twisting activities unless cleared by your therapist or surgeon.
How Can I Maintain A Healthy Joint Long-Term?
Maintaining a healthy joint after hip replacement depends on consistency, variety, and self-awareness. Regular exercise preserves strength and mobility around your replaced joint and reduces the risk of compensatory injuries in other parts of your body. Keep your muscles and supporting tissues strong by alternating aerobic, resistance, and flexibility workouts. Pay close attention to posture, form, and ergonomics during daily activities, especially lifting or bending. Stay at a healthy weight to minimize excess load on your hip, and protect yourself from falls with a home environment clear of tripping hazards. Bull City PT encourages periodic check-ins (annually or as needed) to evaluate gait, flexibility, and strength. This way, your program can be adapted as you age or as your activity levels and health goals change.
What Are The Signs I Should Adapt My Routine For Aging?
Listening to your body is key for long-term rehab after hip replacement. As you age or as other medical conditions arise, pay attention to signals such as increased joint pain during or after exercise, swelling that persists, feelings of instability, or difficulty with balance. If you notice a decline in mobility or the ability to perform exercises that once felt easy, it’s time to consult Bull City PT for a professional assessment. We’ll help modify your routine with alternative exercise formats, introduce supportive devices if needed, or refer you to additional medical care if a new injury or arthritis develops. Open communication keeps you safe while supporting your continued independence and joy in movement.
How Do I Prevent Joint Problems Post-Replacement?
Preventing joint problems after a hip replacement is a lifelong commitment, but with the right guidance, it’s absolutely achievable. Integrate variety into your weekly exercise program and give yourself permission for rest or cross-training if any discomfort arises. Avoid overloading your joints with high-impact sports or heavy lifting unless you have medical clearance. Stay vigilant for any changes in your ability to move, persistent pain, or swelling—these may be signs of joint wear or other issues needing prompt attention. Bull City PT provides ongoing support and education to help you assess your progress and adapt to life’s changes, ensuring that your hip replacement continues to improve your quality of life rather than limit it. Remember, you’re not alone. We’re here for guidance, assessments, and encouragement every step of the way!

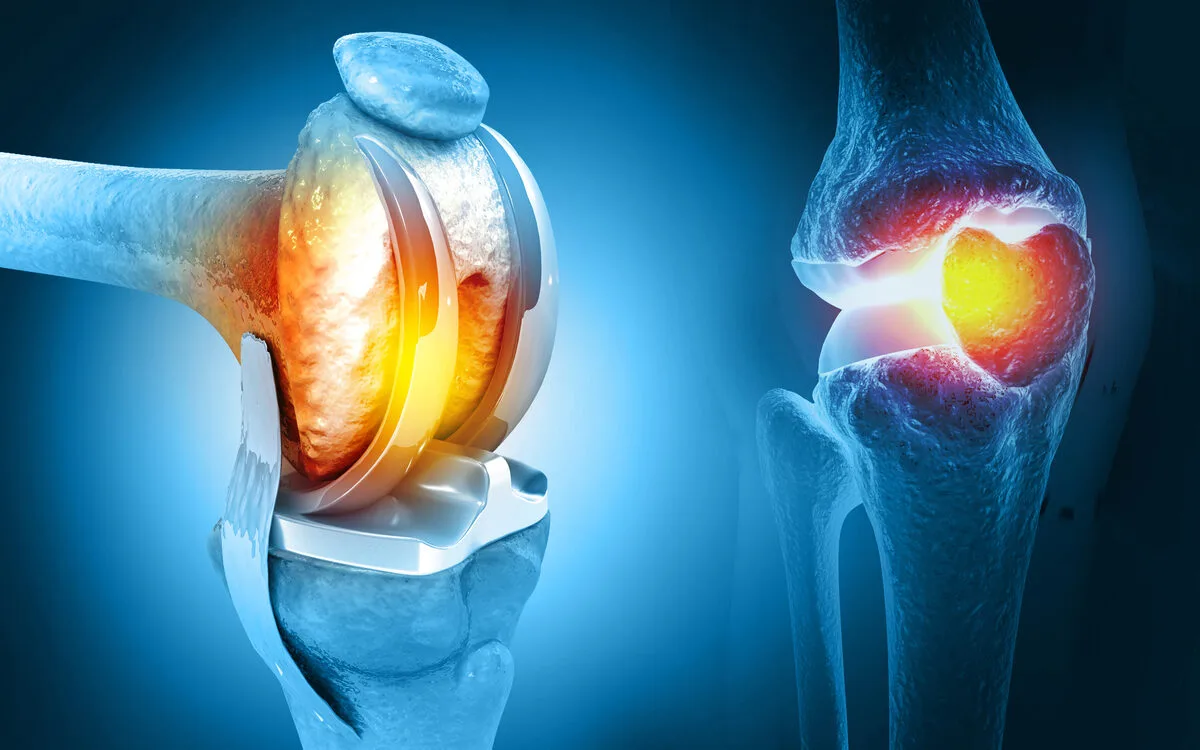
How Many Physical Therapy Sessions After Total Knee Replacement?
Determining how many physical therapy sessions after knee replacement you’ll need depends on your unique recovery journey and individual goals. On average, most patients require between 12 and 24 total knee replacement rehab sessions over 6–12 weeks, though your needs may be more or less based on your progress, health status, and insurance coverage for physical therapy. Many active adults benefit from a combination of hands-on therapy and guidance from their physical therapist, followed by a gradual transition to an independent home program.
What Factors Influence The Number Of Sessions After Knee Replacement?
The precise number of rehab sessions after total knee replacement hinges on several major factors. Your pre-surgery activity level, current strength, age, and any post-operative complications (such as swelling or range of motion limitations) all play a role. Insurance policies, transportation challenges, and your individual progress with prescribed home exercises may also influence how many formal sessions are recommended. At Bull City PT, we work closely with you to set achievable goals and proactively adjust your therapy plan to suit your needs, so you always feel supported and involved.
Should I Continue Exercises At Home After Formal Therapy?
Absolutely! Engaging in a consistent home exercise plan is essential for achieving full functional recovery after knee replacement surgery. While formal therapy is instrumental in guiding proper technique, correcting movement patterns, and ensuring a steady progression, much of your long-term success depends on staying active at home. Your Bull City PT therapist will design a tailored routine for you to perform safely, ensuring you maintain—and continue to build—mobility and strength long after your last session.
When Should I Seek Additional Or Reevaluation Sessions?
It’s normal to have questions or worries during your knee replacement recovery. If you notice increased pain, swelling, difficulty achieving goals, or a plateau in progress, don’t hesitate to reach out for reevaluation. Sometimes, bodies recover at different rates or encounter unexpected setbacks; timely intervention from your therapist can identify and address issues early. Bull City PT encourages open communication—your well-being is our top priority, and we’re always here to ensure your rehabilitation stays on track.
Remember, every recovery journey is unique. Your active participation—both in the clinic and at home—will help you regain confidence, strength, and independence. With personalized support from Bull City PT, you’ll be empowered to return to the activities you love with a strong, resilient knee!
What Is The Best Exercise For Total Knee Replacement?
The best exercise for total knee replacement is often considered to be a combination of movements that build strength, flexibility, and function—most notably, straight leg raises, quad sets, stationary cycling, and heel slides. Each of these exercises targets essential muscle groups that support the new joint, improve your gait, and restore independence.
At Bull City PT, we recognize that every patient’s recovery needs are unique, but strengthening the quadriceps (front thigh muscle) is universally beneficial after a total knee replacement. Straight leg raises and quad sets are foundational because they re-engage the quadriceps without putting excessive stress on the healing knee. These simple, controlled exercises can be done early in your rehab and progressed over time as you gain strength and confidence.
Why Are Quadriceps And Hamstring Strengthening Crucial?
Strong quadriceps and hamstrings protect your new joint and help you regain normal movement patterns. After surgery, these muscles often weaken from disuse or pre-op limitations, making them a primary focus in knee replacement strengthening routines. Quad sets and straight leg raises combat muscle atrophy, while hamstring curls and bridges offer balanced support. This muscle-building not only aids pain-free walking but makes everyday activities—like standing up, sitting down, or using stairs—safer and easier.
Functional Exercises: Getting Up From A Chair And Stair Climbing
Restoring functional strength is key to independence. Practicing sit-to-stand from a chair and stair climbing mimics daily movements, retrains coordination, and builds confidence. At Bull City PT, our therapists integrate these functional exercises for knee replacement into your sessions and teach you how to safely continue at home. We encourage gradual increases in difficulty with supportive equipment as needed, always prioritizing your safety.
Incorporating Exercises Into Daily Routines
Consistency in performing your rehab exercises leads to faster and more sustainable recovery. Incorporate heel slides and stationary cycling into your daily routine—stationary cycling is especially valuable for improving range of motion, circulation, and gentle strengthening. Bull City PT helps you tailor a program that fits your schedule and lifestyle, so you can recover while still managing work, hobbies, or travel.
Preventing Common Post-Op Complications
Regularly performing the recommended exercises helps prevent complications such as stiffness, persistent swelling, or muscle weakness. If you ever notice increased pain, swelling, or difficulty progressing, it’s important to communicate with your Bull City PT team. Our personalized care ensures that you are progressing safely, with modifications as needed, and supports your journey back to the activities you love.
Remember, the best exercise is the one you do consistently and correctly. Partner with the expert therapists at Bull City PT to receive personalized instructions, ongoing encouragement, and hands-on support every step of the way—so you can return to living life to its fullest!
Conclusion And Key Takeaways For Successful Joint Replacement Rehabilitation
Successfully navigating the journey of joint replacement rehab means understanding that recovery is a continuous process, extending well beyond the initial post-surgical phase. By embracing the principles of structured physical therapy, maintaining an active lifestyle, and staying committed to your treatment plan, you can maximize the long-term benefits of your new joint. A thoughtful approach to recovery will help ensure both immediate gains in mobility and strength and lasting improvements to your overall quality of life.
What Are The Keys To Long-Term Joint Health After Replacement?
The foundation of sustained joint health lies in consistency—consistently following prescribed physical therapy routines, integrating safe physical activity into your daily life, and regularly assessing your progress. Stretching and strengthening the surrounding muscles reduces stress on your replacement joint and helps prevent compensatory injuries. Regular exercise types such as walking, cycling, swimming, or light resistance training are excellent for maintaining function and ensuring your joints stay healthy for years to come.
It’s also important to listen to your body. Adjust your activities if new pains or concerns arise, and do not hesitate to reach out for professional guidance. Periodic medical check-ins and consultations with your physiotherapist can catch any early signs of complications or fine-tune your exercise plan, helping you stay ahead of potential problems.
How Can I Stay Motivated Throughout My Recovery?
Staying motivated can feel challenging, especially as initial improvements begin to plateau and daily exercises turn into long-term habits. Goal setting is a powerful strategy—whether it’s walking around the block, returning to your favorite hobbies, or being able to join friends for an outing, meaningful milestones help you stay focused. Celebrate each achievement, no matter how small, and remember these are signs of lasting progress.
Many patients find motivation grows when they have support from family, friends, or a professional care team. At Bull City PT, our compassionate staff not only guides your treatment but also cheers you on every step of the way, helping you overcome setbacks and maintain positive momentum. Regular check-ins, encouragement, and adapting your care plan keep you engaged and invested in your recovery.
Why Is Ongoing Communication With My Physical Therapist Important?
Your relationship with your physical therapist is an invaluable resource in your recovery. PT professionals are trained to monitor progress, address evolving needs, and respond promptly to any concerns. By keeping your therapist informed about your experiences, goals, and lifestyle, you enable them to tailor your program for both immediate successes and sustainable, long-term improvement.
Open communication allows for timely adjustments to your exercises, promotes accountability, and ensures any emerging issues are addressed before they become major setbacks. This partnership is central to achieving and maintaining your optimal joint function and overall well-being.
What Resources Are Available For Continued Support?
After your formal rehab program concludes, you don’t have to go it alone. There is a wealth of community resources—such as support groups, online forums, and local exercise classes—dedicated to individuals recovering from joint replacement. Bull City PT also offers ongoing guidance and periodic assessments to keep you on track. Staying informed with reputable educational materials and maintaining connections with your healthcare team provides you with the confidence and support needed for continued success.
Rediscover the confidence and mobility you deserve with Bull City PT. Our team champions your journey every step of the way, from tailored recovery plans to empowering strategies for active, pain-free living. With personalized care, expert therapists, and ongoing support, we’re here to help you not just recover, but thrive. Start your next chapter in joint health—connect with Bull City PT and experience a partnership that truly prioritizes your goals and well-being.